Immunology
Our immunological studies focus on what provokes autoimmunity. We aim to decipher the deregulated cell types in multiple sclerosis and other neuroimmunological diseases and here in particular T cells and dendritic cells. We want to understand the molecules that serve as regulators of immune cell function and the effector molecules that invigorate an autoimmune response. In addition, learning from evolution, e.g. by understanding how pregnancy and sex differences shape immune responses, will help the quest for novel immunomodulatory treatments for neuroimmunological diseases.

Neurobiology
Inflammatory insults lead to progressive degeneration of axons and neurons that is key for the development of permanent neurological disability in chronic inflammatory diseases such as multiple sclerosis. Our neurobiological studies focus on the molecular mechanisms of this inflammation-induced neuronal degeneration. Stress response pathways can determine neuronal injury, but hormetic stress also stimulates signalling pathways that enhance the abilities of neurons to resist inflammatory stressors. Thus, we aim at discovering conserved molecular pathways that enhance neuronal resilience. Inhibiting damaging pathways or reinforcing protective pathways may lead to the development of novel interventions for neurodegenerative disorders. We aim at identifying, understanding and modulating these key pathways in neurons to ameliorate neurodegeneration in multiple sclerosis and other neurodegenerative diseases.
Systems Biology
Understanding the mechanisms by which neurons alter and maintain their molecular signatures during inflammation is fundamental in understanding their injury. Similarly, autoimmunity changes cellular states by altering gene and protein expression in certain immune cell subtypes. High dimensional readouts such as next-generation sequencing and single cell sequencing, as well as proteomics enable us not only to analyse the complete molecular signatures of cells but also the cascade of events that defines cellular dysfunction or injury. Therefore, we use systems biology to get a comprehensive description of molecular and cellular components and their interactions in neurons and immune cells to predict disease processes (biomarker development) but also to identify novel master regulators of disease, which could be interesting targets for future drug development.
Clinical Research
Based on the concept of health as an ability to adapt to changing personal and environmental settings, clinical research at the INIMS aims to develop treatments with a comprehensive approach. Therefore, clinical care and research includes assessment and consideration of psychological and psychosocial aspects of multiple sclerosis as well as educational (i.e. evidence-based patient information), behavioural (i.e. psychological) and lifestyle (i.e. exercise) interventions. Moreover, we pursue phase I and phase II treatment trials combined with mechanistic laboratory studies in the area of unmet clinical needs such as safe treatments in early MS (i.e. boswellic acids, immunological tolerance induction), highly immunosuppressive approaches for aggressive MS (i.e. autologous hematopoietic stem cell transplantation) but also neuroprotective concepts (i.e. erythropoietin). Complementing this approach, we conduct research to improve assessment tools, develop novel outcome parameters with clinical relevance, and optimize study designs.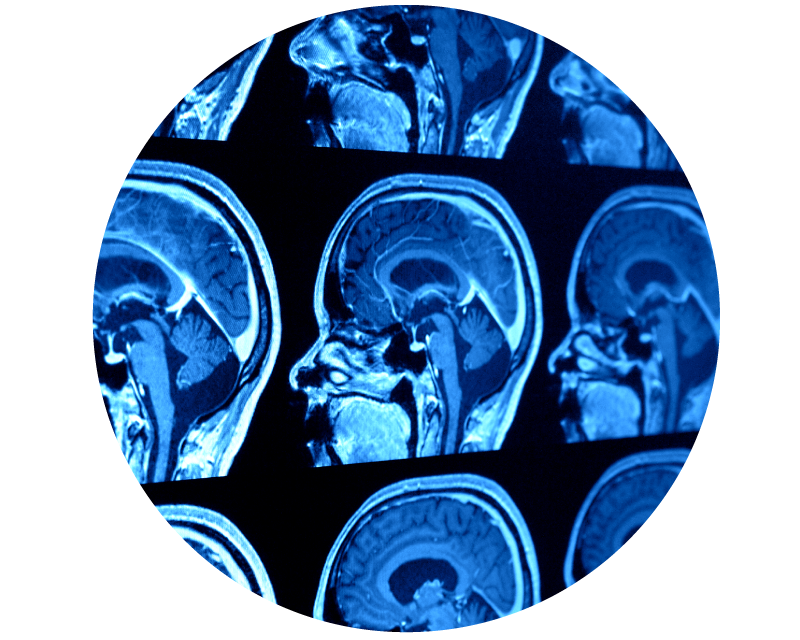
Imaging Research
Magnetic resonance imaging is the most promising approach to monitor subclinical disease activity in several neurological diseases including multiple sclerosis. At the INIMS, we aim to improve the understanding of integrity, structural and functional organisation of the brain and its adaptive or regenerative mechanisms by developing and validating new imaging techniques. Natural history cohorts and randomised controlled trials provide an ideal and translational framework to establish such techniques as a methodical link between disability progression and the underlying pathology. Moreover, multiple sclerosis can be seen as model disease that instructs our understanding of the structure and functional organisation of the healthy brain. Further research activities include the development of new post-processing algorithms, as well as the investigation of Optical Coherence Tomography (OCT) as an additional imaging method of neurodegeneration.